Answer: The APRN Consensus Model is a model outlining recommendations for uniform regulations for APRN licensure, accreditation, certification, and education (collectively known as LACE) across all states in America. The Model’s core objective is to unite the public, medical practitioners, and state and national legislatures in their understanding of the APRN’s role, with the intent to support APRNs’ ability to practice to the full extent of their training and qualifications.
The National Council of State Boards of Nursing (NCSBN) APRN Advisory Committee and the APRN Consensus Work Group first developed the APRN Consensus Model in 2008. This Model is the product of a series of discussions around defining the role of the advanced practice registered nurse and outlining the different educational and clinical standards APRNs must meet in order to earn national certification, state licensure, and scope of practice privileges.
The APRN Consensus Model defines certification as “the formal recognition of the knowledge, skills, and experience demonstrated by the achievement of standards identified by the profession,” and states that certification is distinct from licensure, which is the “granting of authority to practice.” National certification through organizations such as the American Nurses Credentialing Center (ANCC), the American Academy of Nurse Practitioners Certification Board (AANPCB), and other accredited certifying bodies is a requirement for licensure, which occurs at the state level.
The APRN Consensus Model aims to unite nursing programs, state boards of nursing, and national certification organizations in their definition of the role of the APRN so that nurses who wish to become APRNs face the same standards across states and throughout their education and applications for certification and licensure. As APRN licensure and scope of practice is determined by state boards of nursing and other legislative parties at the state level, APRNs can face barriers that interfere with their ability to practice to the full extent of their training. For example, if an APRN moves states, he or she must meet different licensure requirements for each state in which they practice. In addition, the lack of standardization across the states has made expanding APRNs’ scope of practice more difficult, as each state that does not grant APRNs full practice authority must individually change laws to broaden nurses’ practice privileges. The APRN Consensus Model seeks to address these and other issues by establishing standard definitions and mandates for APRN licensure and practice.
To help current and prospective APRNs better understand the APRN Consensus Model and its recommendations, we have outlined several of its key recommendations below.
Define the Four Categories of APRN
The Consensus Model outlines four categories of APRN: nurse practitioners (NPs), clinical nurse specialists (CNSs), certified registered nurse anesthetists (CRNAs), and certified nurse midwives (CNMs). The model defines these clinical roles as such:
Nurse Practitioners
Nurse practitioners diagnose and treat patients across the continuum of care, and provide physical examinations and health assessments, diagnostic screenings, treatment of acute and chronic conditions, care coordination, and patient case management. Their duties include ordering, supervising, performing, and interpreting laboratory tests and imaging; prescribing medications and durable medical equipment; making patient referrals as needed; and educating patients and their families. Depending on their population focus, NPs may work with individuals across the lifespan in family care, pediatrics, geriatrics, internal medicine, and acute care settings such as the emergency room and trauma units.
Clinical Nurse Specialists
Clinical nurse specialists work to improve patient outcomes at the individual patient and system levels through mentorship of nurses, patient education, and evaluating and streamlining systems of care. According to the Model, CNSs have a unique role that “integrates care across the continuum and through three spheres of influence: patient, nurse, system.” They are responsible for patient diagnoses, management and treatment of disease, health promotion, and illness prevention through education and support of individuals, families, groups, and communities.
Certified Registered Nurse Anesthetists
CRNAs provide full-spectrum anesthesia care to patients across the lifespan and across the spectrum of health statuses, from normal/healthy to life-threatening illness or injury. CRNAs are trained to provide this care in diverse medical environments, including hospital surgical departments, obstetrical departments, palliative care centers, ambulatory surgical centers, and the offices of dentists, plastic surgeons, podiatrists, and ophthalmologists.
Certified Nurse Midwives
Certified nurse midwives provide a full range of primary and reproductive health care services to women throughout the lifespan, including gynecological care, family planning, preconception counseling and care, support during labor and delivery, postpartum care, and infant care. CNMs work in patients’ homes, hospitals, birth centers, ambulatory care settings, physicians’ private practices, and community health clinics.
Establish Population Foci for Certification and Licensure
Within the four roles described above, the Model designates six “population foci” that state boards of nursing and national certification organizations should use to structure their licensure and certification requirements:
- Family/Individual Across the Lifespan: The primary care of patients across the lifespan, with an emphasis on supporting the health of the family unit through individual patient care.
- Adult-Gerontology: The primary or acute care of adult patients ranging in age from young adulthood to geriatric age.
- Neonatal: The care of moderately to acutely ill neonates in the neonatal intensive care unit (NICU) as well as related settings such as step-down nurseries.
- Pediatrics: The primary or acute care of pediatric patients in settings such as hospitals, private offices, or the pediatric intensive care unit (PICU).
- Women’s Health/Reproductive Health: The primary and reproductive care of women from adolescence through menopause.
- Psychiatric Mental Health: The evaluation and care of patients’ mental, emotional, and behavioral health in settings such as outpatient behavioral health clinics, inpatient psychiatric units, private practices, and community health centers.
The Model recommends that APRNs be trained and licensed according to their role and population focus, and does not recommend that APRNs be licensed in specialties that are not within the aforementioned population foci, such as palliative care, oncology, or substance abuse. However, APRNs can specialize in these areas after receiving training and earning national certification and state licensure for a designated population. For example, an RN can receive training and earn both certification and licensure as a Family Nurse Practitioner, after which he or she could specialize in palliative care, nephrology, or corporate health nursing, but would not receive certification in these areas.
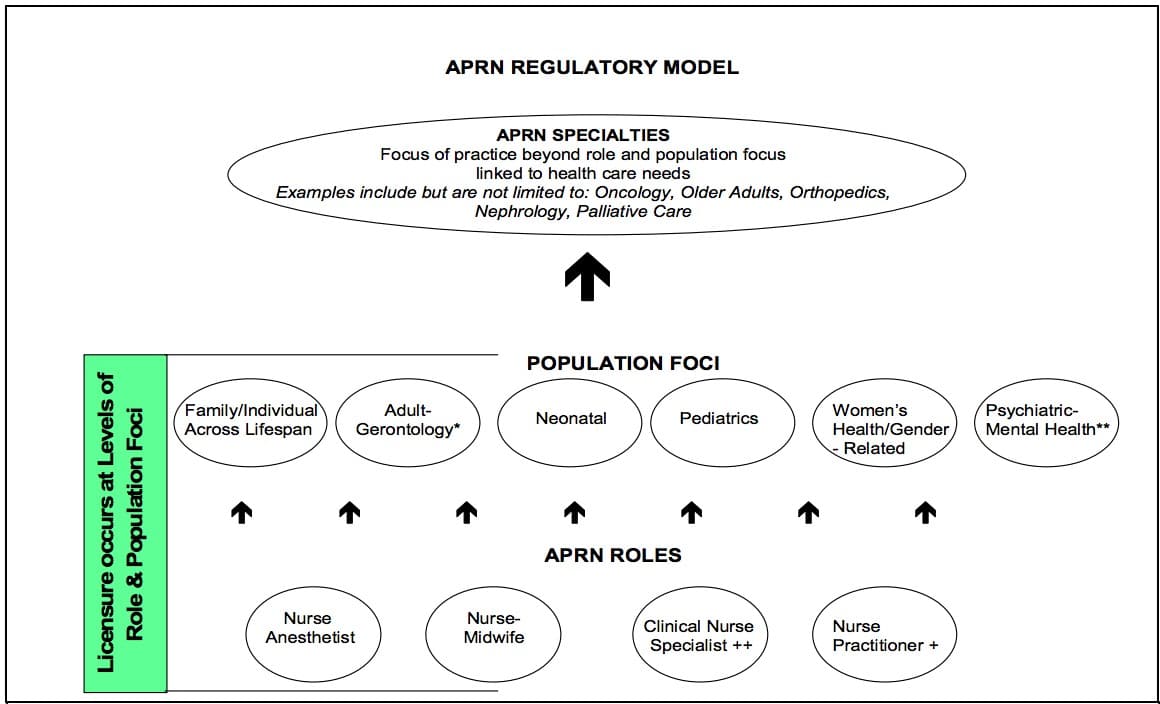 “Image from “Consensus Model for APRN Regulation: Licensure, Accreditation, Certification & Education,” ncsbn.org, National Council of State Boards of Nursing, https://www.ncsbn.org/Consensus_Model_for_APRN_Regulation_July_2008.pdf
“Image from “Consensus Model for APRN Regulation: Licensure, Accreditation, Certification & Education,” ncsbn.org, National Council of State Boards of Nursing, https://www.ncsbn.org/Consensus_Model_for_APRN_Regulation_July_2008.pdf
Establish Educational Requirements for Certification and Licensure
According to the Model’s recommendations, to earn national certification and state licensure, APRNs must complete a graduate nursing program that has been accredited by a nursing or nursing-related accrediting organization recognized by the U.S. Department of Education and/or the Council for Higher Education Accreditation. Most graduate nursing programs are accredited by one or both of two nationally recognized accrediting organizations: the Commission on Collegiate Nursing Education (CCNE) and the Accreditation Commission for Education in Nursing (ACEN).
During their graduate program, prospective APRNs must complete comprehensive post-baccalaureate classes in advanced physiology and pathophysiology, advanced health assessment, and advanced pharmacology, as well as graduate-level content that is specific to their role and their population focus or foci. In addition to academic work, graduate nursing students must complete sufficient clinical experience in order to be eligible to sit for national certification examinations and apply for state licensure. After they have earned the necessary credentials to practice as APRNs, individuals must still participate in continuing education to ensure ongoing competence.
The APRN Consensus Model’s Impact on Nursing Education and Credentialing
The APRN Consensus Model has received the endorsement of 41 nursing organizations, and has been adopted in part by several state boards of nursing in their creation and revision of policies outlining APRN licensure requirements and scope of practice. In addition, several states have used the Model as a basis for updating their scope of practice licensure regulations for NPs, CNSs, CNMs, and/or CRNAs practicing in their state. While the goal for full adoption of the Consensus Model across all state boards of nursing was 2015, as of 2017, numerous states are still working to incorporate the Model’s definitions and recommendations into their legislation.
The Model has had a significant impact on national APRN certification organizations. The American Nurses Credentialing Center recently consolidated and streamlined their certification options for nurse practitioners and clinical nurse specialists, updating their certification requirements to reflect the recommendations outlined in the Model. The ANCC retired its Acute Care Nurse Practitioner, Adult Nurse Practitioner, Adult Psychiatric Mental Health Nurse Practitioner, and Gerontological Nurse Practitioner certifications, and now offers certifications that align with the APRN Consensus Model: Adult-Gerontology Acute Care NP, Adult-Gerontology Primary Care NP, Family NP, Pediatric Primary Care NP, and Psychiatric-Mental Health NP.
The American Academy of Nurse Practitioners Certification Board (AANPCB) also decided in 2012 to create an Adult-Gerontology Primary Care Nurse Practitioner certification starting in 2013, and retire their Adult Nurse Practitioner and Gerontology Nurse Practitioner certifications. The American Association of Critical Care also updated their certifications, retiring its Adult Acute Care NP, Adult Acute/Critical Care CNS, Pediatric Acute/Critical Care CNS, and Neonatal Acute/Critical Care CNS certifications and awarding the following new certifications: Adult-Gerontology Acute Care NP, Adult-Gerontology CNS, Pediatric CNS, and Neonatal CNS.
It is important for current and prospective APRNs to stay updated on any new requirements for national certification in their role and population focus of choice, and to keep their national certifications current once they pass their certification exams. Furthermore, they should check with their state’s board of nursing to see if any changes have been or will be made to the licensure requirements they must meet to practice in their state of residence. While the Model has taken time to implement and has led to the retirement of some national certifications in certain APRN specialties, it has helped clarify the role of the APRN, ensured that APRNs receive sufficient training to ensure patient safety, and established standards that reaffirm APRNs’ qualifications to serve patients independently in a wide variety of medical environments.
Sources:
- “Consensus Model for APRN Regulation: Licensure, Accreditation, Certification & Education,” ncsbn.org, National Council of State Boards of Nursing, https://www.ncsbn.org/Consensus_Model_for_APRN_Regulation_July_2008.pdf
- “FAQ: Consensus Model for APRN Regulation,” nursecredentialing.org, American Nurses Credentialing Center, https://www.nursingworld.org/certification/aprn-consensus-model/faq-consensus-model-for-aprn-regulation/
- “National Certification Expectations for Entry-Level NPs,” aanp.org, American Association of Nurse Practitioners, https://www.aanp.org/education/student-resource-center/starting-your-career/9-education/1060-certification-for-entry-level-nps
